|
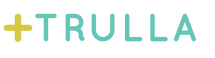
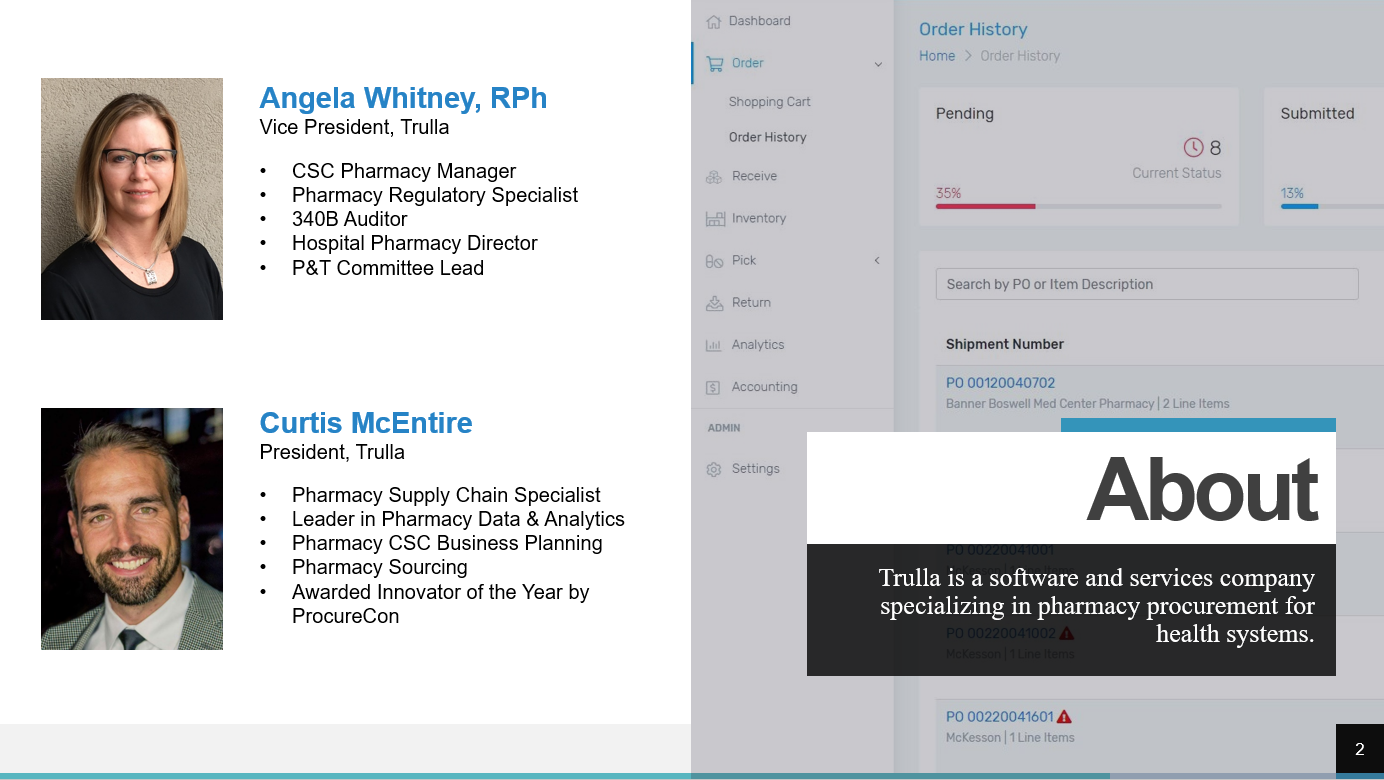
It was the year 2012, I had been working in hospital pharmacies for over 22 years and felt like I had done it all. But then I was exposed to a new challenge: manage the pharmacy operations of our health system’s consolidated service center (CSC). We built our CSC with the purpose of better managing inventory, reducing expired medications, taking advantage of strategic purchasing, repackaging, and sterile and non-sterile compounding. Those all had clear value propositions that we had anticipated. The one activity that completely surprised me was providing pharmaceuticals and pharmacy support to our 300+ clinic locations. Conventionally, clinics receive minimal support and information regarding the medications on formulary, purchasing contracts, suppliers, shortages and management strategies, and the quantities and cost of expired drugs from that location. Often pharmacies within a health system are tasked with supporting the clinics but do not have systems to support this service. Processes are generally developed that minimally meet the need with limited ability to communicate directly with those purchasing pharmaceuticals. Most clinics receive their pharmaceuticals from the health system’s CSC, a nearby hospital pharmacy, or from a distributor like Henry Schein. Take note that it is typical for a clinic distributor to charge a “cost-plus” model while the hospitals are buying the same medications from their primary distributor in a “cost-minus” model. The swing for clinics to purchase most medications through their hospital pharmacy can be close to 10% in savings! For clinic orders to a CSC or hospital pharmacy, the orders often arrive via email, fax, or even a paper requisition that may be hand-delivered to the pharmacy. If the department or clinic is to be charged for the products, then a manual process of entering the transaction information (e.g., drugs, quantities, cost) into a spreadsheet or other program for tracking follows. The transaction information is the submitted to finance periodically to initiate journal entries. At the clinic, drugs are received and accounted for via a few different mechanisms varying in formality. Some clinics simply look through the delivery and restock the drugs while others may be required to sign a paper order to indicate the products were received which is returned to the pharmacy. There is plenty of room for things to slip through the cracks with these manual, disjointed processes. To address the issues described, a health system should consider obtaining a procurement system that will capture cost savings and simplify the ordering and fulfillment processes for their clinics. Finding a solution that addresses both the needs of those procuring pharmaceuticals and those fulfilling the orders can be challenging. Solutions have not historically been aimed at solving this problem. This is one of the reasons we developed Trulla, a pharmacy procurement system built for the entire health system, hospitals, and clinics. Trulla provides valuable information at the point of ordering simplifying the experience for the individual while standardizing purchasing and concurrently capturing cost savings for their clinic. The solution efficiently guides them to purchase the preferred product from the preferred supplier each time with real-time product selection. The ordering process is the same whether the supplier is a hospital pharmacy, a CSC, a wholesaler, or a manufacturer. Trulla can also present a limited list of drugs to the user…only those that they are authorized to buy for patient safety and efficiency, with the ability to create templates easily for even faster ordering. For fulfillment, the system provides pick lists, shipping manifests, and automatic journal entries with updated pricing. For the clinic staff, the receiving process is effortless and supported electronically to improve tracking and accountability. Utilizing a simple, efficient, and cost-effective solution to standardize purchasing for clinics will put smiles on the faces of both the clinic and pharmacy staff and will add time to their day! Angela Whitney, RPhAngela serves as COO for Trulla. She is a 340B ACE and has worked as a Director of Pharmacy, Manager of Pharmacy Operations at a Consolidated Services Center, and other pharmacy roles within a health system.
0 Comments
Consolidated Service Centers (CSCs) centralize many pharmacy services along with the inventory of a health system and capture significant savings through processes such as strategic buys, standardization, and low units of measure distribution, just to name a few. But the most frequently asked question by health systems implementing a CSC is: “How can I compliantly ship medications to my 340B covered entities and make it so they can still utilize their available 340B and GPO accumulations?
It becomes increasingly difficult to distribute drugs from a central location when the health system includes one or more 340B covered entities (CEs). Those of us who have worked in the 340B world understand that this is due to the complex rules and regulations covered entities must abide by along with the associated risks if found non-compliant. It is critical for health systems to tackle this problem because the advantages of a consolidated service center are drastically reduced if they are not able to ship products to their CEs. For those of you evaluating the options surrounding central distribution and CEs, or for those of you looking to optimize, please allow us to share some of the observations and lessons learned along the way to becoming the leading team in the industry: Should I just have a separate inventory? Most who consider maintaining separate inventories quickly recognize space will be an issue. There are also serious concerns that multiple inventories would be more difficult to manage and pose a risk that orders will be picked from the wrong inventory, exposing you to 340B compliance violations. A combined inventory is more optimal. Can I just purchase everything at my CSC on WAC? You can purchase all your CSC inventory at WAC both initially and ongoing. The advantage of this approach is that you can compliantly ship to both CE and non-CEs and avoid additional tracking at the CSC. However, purchasing strictly at WAC would significantly increase the cost to the health system, limiting the number of products stocked, services offered, and value of your CSC. What if I purchased everything at GPO? You can choose to just have your CSC purchase strictly at GPO. This inventory could be provided to non-CEs and those CEs that are not subject to the GPO prohibition without additional tracking at the CSC. However, CEs subject to the GPO prohibition would only be able to purchase from the CSC if they have GPO accumulations. For any CE to take advantage of their 340B accumulations and purchase at the lowest cost, they would be required to place orders with their wholesaler or another direct vendor, bypassing the CSC. With this option, the CSC would not be the sole supplier of a product which would impact inventory turns and potentially the product dating. A WAC or GPO based inventory that utilizes the accumulations of the covered entities for replenishment, rather than ignoring them, further reduces overall costs to the health system. Although maintaining a GPO based inventory is clearly the lowest cost, it requires a complex tracking process to maintain compliance. The upside of this approach is that the entire health system can utilize the centralized services and the products stocked at the CSC. CSCs are also able to function as the sole supplier of a product resulting in increased inventory turns, improved product dating, and less waste due to expiration. Everyone who has started down the path of having a GPO inventory with accumulation-based replenishment ends up developing complex manual processes to maintain the compliance of their several CEs. The highest value is with this approach, but the tracking is tedious and next to impossible to manually manage compliance or the inventory levels at the CSC. What is the best solution? Trulla has developed a patent pending procurement solution that enables CSCs to compliantly distribute medications to your CEs while utilizing available 340B and GPO accumulations to maximize their savings. Utilizing a robust 340B compliance engine inside Trulla’s pharmacy procurement software, health systems can maximize savings and ensure compliance when shipping medications from their CSC. Contact us at [email protected] to schedule a demo and learn more. Are you considering a pharmacy CSC (consolidated services center) for your health system? This recorded webinar dives into what you need to know when considering a pharmacy CSC. Learn what services you should consider, challenges o watch out for, 340B complexities, licensure, and more!
This webinar is presented by Angela Whitney, RPh and Curtis McEntire, who have been integral in the planning and operations of multiple pharmacy CSC's around the country. Click here to access the webinar. How much does the drug you’re dispensing actually cost and are you buying it at the best possible price? Did you know that for every medication that is generically available there is an average of 13 NDC’s that can be purchased? With drugs and drug prices constantly changing, knowing which NDC to order and utilize is complex for even the most experienced pharmacy buyers. Contractual agreements supported by rebates, administrative fees, or 3rd party programs can cloud what on the surface seems like an easy question – is this the NDC I should buy? In pharmacy, it’s so complex to analyze and review the true pricing, not to mention trying to couple that analysis with current and historical utilization, tier thresholds, and other variables. It’s even harder when you consider that most of the “tools” we do have access to are in multiple, disparate, manual solutions. Add in the variables of the 340B Program requirements and other clinical-based programs and you soon realize how difficult, if not impossible, it is to guide purchasing within even the smallest inpatient pharmacies, let alone across an entire health system, a growing number of which include a central distribution operation. The tragedy is that we all understand that standardizing to the best NDCs and suppliers for your organization can bring significant benefits both clinically and financially. Having a software solution which can ingest utilization and purchasing data from your suppliers and communicate with those suppliers can sharply improve the benefits for an organization. Imagine being able to identify and control the NDCs to order at a health system level by leveraging the preferred logic and the settings available in the Trulla Procurement Software. This ability will drive several benefits to the health system which includes:
By leveraging the analytics derived from current spending patterns and the software which can set default, preferred NDCs, Trulla is uniquely positioned to identify your best opportunities and deliver results by allowing leaders to easily implement decisions across your health system. The impact of Trulla is amplified as health systems become increasingly complex. Trulla’s software is specifically designed to enable the selection of preferred NDCs to meet the needs of corporate and/or local initiatives and to continuously guide users throughout the procurement process. Finally, the industry has a tool to not only direct you to savings within your pharmacy spend, but to implement decisions and track the benefits they deliver! Isn’t it time to maximize your pharmacy savings? Formulary management. There are few words found within the pharmaceutical lexicon that elicit as much joy and exuberance as “formulary management”. If you think that’s even remotely true, you must be new to formulary management. With the (thankfully) increasing opinion that a health system should operate more like an actual system, the dire need for proper and auditable formulary management is becoming increasingly evident. We can’t run a diverse health system with a one-size fits all approach and we also can’t efficiently serve our patients if we persist in the historical “every facility an island” approach. Across the industry, we just don’t see good auditing tools to ensure that we’re purchasing the correct, optimized pharmaceuticals. We’ve spoken previously about the unsung hero, the pharmacy buyer, and we can really give them and their clinic counterparts a leg up by handing them a tool that ensures proper formulary management and compliance.
There are lots of reasons why system-wide formulary management is complicated: hospital vs. clinic, patient populations, the 340B Drug Pricing Program, different regional needs, supplier access, and so on. The list of why there hasn’t been a good solution to this is much shorter: no one that truly understands the industry has built a comprehensive tool for the industry, until now. Trulla enables users to operate from the broadest sense (all active medications for an entire health system) to the absolute most narrow sense (the 15 medications that a seasonal shack on the backside of a mountain might need access to). The way that Trulla approaches formulary management is novel in a few ways, not the least of which is that we recognize and respect that there are medications that a health system may need that they don’t want everyone purchasing at will and that the pharmacy buyer can never be replaced; they need the freedom to be able to purchase beyond machine-driven logic. Trulla operates as a funnel to present a buyer with the optimized product, specific to their department and health system, but we don’t lock them into that product. At the widest point of the funnel, we have access to all active medications with the FDA so that those managing the formulary don’t have to build each medication profile from scratch. The next step in the narrowing funnel includes on formulary and off formulary medications, restricted medications, and so on. As we narrow the funnel even more, Trulla allows for the restriction of a visible sub-formulary as it pertains to each buyer and their location. Let’s say there’s a system-level decision made by the P&T Committee, or the 340B team has new information about where to purchase X medication from to realize the best compliant price, Trulla allows for the operationalizing of that information. A 340B clean site will see only those medications that they should have rights to purchase. A non-340B clinic may see a broader sub-formulary but still doesn’t have access to everything an inpatient pharmacy would have access to, and so on. Proper formulary management, coupled with a tool to operationalize it, creates an environment where even the administrative assistant at a clinic who’s thrown into a one time only purchasing situation can see the same results as the most experienced hospital buyer. Your goal is to save time and money while keeping patient safety at the forefront of every decision. Formulary management may not be the first thing that comes to mind when thinking about saving time and money, but let Trulla show you a new angle that’s afforded by our software. With the Trulla software you’ll have access to a ready-to-go, customizable medication list to begin building a broad formulary that serves as a source for any number of sub-formularies for those who purchase pharmaceuticals. With our tools, you’ll have a united front all the way across your facility or health system, working together towards the same goals. Many healthcare systems are creating Consolidated Service Centers (CSC) to help standardize the pharmaceutical experience throughout their system. There are many cost savings and quality improvement benefits to consolidating pharmaceutical practices. Unfortunately, when it comes to centralizing sterile compounding there is a great deal of misunderstanding when it comes to registering with the FDA; specifically, whether to be a state regulated 503A or an FDA regulated 503B. The most common notion is that registering as a 503B is the right approach. Even though that approach might appear to be the safest option, registering with the FDA as a 503B outsourcing manufacturer is not the same thing as operating an inpatient pharmacy following the standard USP 797 regulations. It is better to think of 503B as becoming an actual manufacturer with its own set of rules. To be effective, selecting the 503B path would require a different business model to cost justify such an operation. Fortunately, working within the confines of the 503A classification can still produce a quality product for patients and help keep the high costs associated with Current Good Manufacturing Practice (CGMP) from disrupting certain aspects of a consolidated services approach.
The draft guidance for Hospital and Health System Compounding Under the Federal Food, Drug, and Cosmetic Act: Guidance for Industry dated April 2016 states, “…FDA does not intend to take action if a hospital pharmacy distributes compounded drug products without first receiving a patient-specific prescription or order provided that: (1) The drug products are distributed only to healthcare facilities that are owned and controlled by the same entity that owns and controls the hospital pharmacy and that are located with a 1 mile radius of the compounding pharmacy;” Forcing CSCs to register as 503B because they move compounded product more than 1 mile from the facility that compounded the product is frequently misinterpreted and does not align with the regulations which clearly allow for anticipatory compounding and interstate distribution of products when certain conditions are met. It is important to focus on the applicable statutes and regulations as found in Section 503A of the Federal Food, Drug, and Cosmetic Act. The guidance documents have limited ability to be enforced when they make statements and claims outside of the applicable statutes and regulations. To reinforce this, many of the Guidance for Industry documents contain in their introductions: “You can use an alternative approach if it satisfies the requirements of the applicable statutes and regulations.” The headers on many of the pages within the documents also state: “Contains Nonbinding Recommendations.” The key requirements for maintaining 503A compliance for most CSCs are as simple as:
CSCs are in a unique position to receive valid prescription orders for identified individual patients. With the advancements in electronic health records, CSCs can operate as a member of their health system with full access to required documentation and the ability to generate auditable reports to support their practice. Section 503A and the FDA guidance documents have left opportunities for healthcare systems to take a defensible position on identifying their CSC(s) as 503A. Consolidating sterile compounding can increase safety and decrease costs for patients without taking on the unnecessary burdens of registering with the FDA as a 503B outsourcing manufacturer. Centralized Services Centers have been implemented or are being considered by numerous health systems to improve efficiency, reduce medication errors, and for the potential cost savings that can be captured. However, inventory management is extremely challenging when the Centralized Services Center (CSC) provides medications to both non-covered and covered entities (CEs). Ensure that the inventory management model selected does not expose the CEs to a GPO prohibition violation if they are required to comply with this requirement.
For example, some health systems have centralized the sterile compounding of products such as TPN and various antibiotics. If any of these products are administered to covered outpatients and purchased on GPO by the CSC, the CE could be at risk for a GPO prohibition violation unless a strategy is in place to prevent this from happening. The 2013 HRSA 340B Drug Pricing Program Notice Release No. 2013-1, Statutory Prohibition on Group Purchasing Organization Participation states, “Organizations that are not part of the 340B covered entity are not subject to the GPO prohibition; however, the 340B covered entity is still prohibited from having organizations purchase covered outpatient drugs through a GPO on its behalf or otherwise receive covered outpatient drugs purchased through a GPO.” One of several strategies to consider is to place these compounded products on a non-covered outpatient drug list. With this approach, they can be excluded from the 340B program and will not be subject to the GPO prohibition. The downside to this approach is that the individual ingredients cannot be purchased on 340B which could result in lost savings. If your health systems needs help determining a compliant approach, you can find a team of experts at Trulla (www.trullarx.com) or reach out to them directly by emailing [email protected].  There are various reasons to centralize targeted inpatient pharmacy services. Some of the reasons include process standardization, increased efficiency, medication safety, and the ability to capture cost savings for the company. Sterile, non-sterile, and hazardous compounding services typically top the list of services that are often consolidated. Other services that are centralized include packaging, low unit of measure distribution, cart fill, kit processing, medication order entry, contracting, buying, shortage management, and general pharmacy services for clinics within the system. How do you know what services make sense for your hospital or health system to centralize? It can be extremely difficult to fully understand the opportunities associated with a centralized service as well as the obstacles that will need to be faced in order to effectively take advantage of the prospect. We have assembled a team of experts, with this need in mind, that have first-hand experience centralizing a variety of pharmacy services. This diverse team can conduct an in-depth analysis of your hospital or health system to identify both improvement and cost savings opportunities. In addition, they can provide guidance on the best implementation strategy. Some hospitals or health systems will best be served by a consolidated service center while it may be most advantageous to use a hub and spoke model at others. With a well-designed business model which leverages the health systems’ investment in automation and highly trained personnel, consolidation will result in quality products and pharmacy services for the patients that are served while saving the company money. If you would like to learn more about what Trulla has to offer, please reach out by sending an email to [email protected]. In today’s environment, creating Centralized Service Centers (CSCs) to standardize medication processes, increase efficiency, improve safety, and to save money is quickly becoming a reality for many health systems. Centralized packaging, sterile and non-sterile compounding, and targeted purchasing allows the individual sites in a health system to order EXACTLY what they need instead of being forced to order the pack size available from the manufacturer. These services reduce the workload at the sites, the medication outdates and waste, along with the cost associated with each of these activities. Highly trained individuals that are working in an environment free from interruptions reduces errors and improves medication safety. It is easy to see why this is appealing to health systems as these CSCs have the ability to serve several inpatient pharmacies and outpatient clinics simultaneously.
Since this industry is moving so quickly in this direction, it is easy to forget that centralizing the services that involve controlled substances can be tricky and must be managed carefully. Remember, that the five percent rule remains in effect for CSCs that are registered as a hospital/clinic with the Drug Enforcement Administration (DEA). What this means is that the total number of dosage units of all controlled substances distributed by a pharmacy may not exceed five percent of all controlled substances dispensed by the pharmacy during a calendar year. If at any time the controlled substances distributed exceed five percent, the pharmacy is required to register as a distributor. In addition, if the controlled substances are manipulated, such as being repackaged or used in compounding, the pharmacy may also need to register as a manufacturer. To add to this burden, distributors and manufacturers have additional record keeping and reporting requirements when compared to a pharmacy. Remember, it is critical to have the correct DEA registrations in place BEFORE providing centralized services that involve controlled substances! If your health system needs experts to evaluate the activities of their CSC or to analyze their controlled substance compliance, please email [email protected]. With the grouping of hospitals into health-systems, we are seeing more and more central distribution centers being created to leverage the purchasing power of the group. However, there are many options for what services can be provided, and some are more beneficial than others. It is a case of good, better, or best decisions, and of course there are just some bad decisions. Our team has hands on experience in planning, creating, managing, and leveraging these processes, and we can share this experience with you to ensure you are maximizing your savings sooner than later.
|
ARCHIVES
March 2022
Categories
All
Disclaimer: The information provided in this article does not constitute legal advice and should not be construed as such. Readers of this document are encouraged to contact their attorney to obtain advice with respect to any particular legal matter. The views expressed in this document are those of the author and not those of the Trulla LLC. All liability with respect to actions taken or not taken based on the contents of this document are hereby expressly disclaimed. The content in this document is provided “as is;” no representations are made that the content is error-free. |
Contact us to help you optimize your pharmacy procurement. |
E-mail: [email protected]
|





 RSS Feed
RSS Feed